
Norfolk charity comforts the dying in Ethiopia
Ethiopia has one hospice for a population of 112 million. Half of its funding comes from a charity led by Sue Mumford, a nurse who lives in north Norfolk.
“My doctor husband and I are really privileged to have found a passion,” said Sue, “and fortunate that we can do this together. And we are in good enough health to cope with the rigours of travelling in Ethiopia.”
Sue is a Community Specialist Palliative Care Nurse. She helps people cope with the end of life, by controlling pain and symptoms, and offering psychological and spiritual support.
“Dying is a really distressing time for patients and their families,” she said.
Her husband Jamie is a GP at Aylsham with a special interest in palliative care, so they make an ideal team.
Sue is part of the extended Gurney family, the distinguished Norfolk banking family. One of her childhood friends was her cousin Pippa, now Lady Pippa Dannatt, Lord Lieutenant of Norfolk, who is a keen supporter of the work of Hospice Ethiopia.
Sue traces the beginnings of her mission to meeting Dame Cicely Saunders during her training at Barts in London. Following a year nursing in Switzerland she returned to England where she cared for patients with lung cancer on a respiratory ward at Papworth Hospital, and started asking herself how to provide the best care for them.
It was at this time that she met Jamie, at that time a glaciologist. They decided to move together to Oxford, where he retrained in medicine.
Their first opportunity to see medical care beyond the abundance of the United Kingdom came when Jamie chose to do his elective in India. “It was a real eye-opener,” said Sue. “Only three of the patients in the hospital where we were working had pain killers.”
After her husband settled down as a GP in Aylsham, she volunteered at Priscilla Bacon Lodge in Norwich, which provides end-of-life care to patients with life-limiting illness. However, staff soon spotted that she was trained, and persuaded her to do the return-to-nursing course. She subsequently gained a Degree in Nursing at the University of East Anglia. Part of her course enabled her to become a nurse prescriber which proved invaluable in her later work.
Meanwhile Dr Katie Carpenter from Priscilla Bacon Lodge was developing a twinning arrangement with Hospice Ethiopia, which had been founded in 2003 by a nurse called Tsigereda. The idea was that the two hospices would share staff and expertise. It soon became apparent, however, that what was most needed were funds (as they receive virtually no funding from within Ethiopia) and as the nurses had been well trained in palliative care at Hospice Africa Uganda in Kampala.
In 2012 Sue was part of a group which went out to Ethiopia to visit the twin, and she started to recognise the enormous need.
“Poor people in Ethiopia get free admission to hospital,” she said, “but treatment costs money. So it is beyond them.”
Hospice Ethiopia provides care for people in their own homes. It gives out medicines, catheter bags, stoma bags and dressings (donated by foreign healthcare professionals) free of charge. After giving a means test, it may also provide food and other essential items for patients, who sadly are often abandoned by their partners.
One memorable patient Sue met was a woman who had breast cancer, and who was being cared for by her teenage daughters after her husband had left her. She visited the patient every couple of weeks, got the pain under control and made sure there was food in the house. Towards the end of her stay in Ethiopia, the woman, who previously had refused to be photographed, asked if she could have her picture taken.
“In some ways palliative care is harder in Ethiopia,” said Sue. “Often there is no point in sending people to hospital because none of the treatments such as radiotherapy will be available or will cost too much. But in some ways, it is easier. In the UK, people might use their final weeks trying six or seven treatments, none of which is particularly effective. Sometimes it’s best not to have a myriad of options, but just to have the time to sort out one’s affairs and enjoy precious time with friends and family.”
In both countries the essential mission is the same: maximising the quality of life, calming the situation down, finding some areas of pleasure, and coming to terms with what is happening.
The team at Hospice Ethiopia UK pay all their own travel and hotel costs, and a local business covers the administrative costs. So all money donated goes to the hospice in Ethiopia. The main need is staff salaries. There are also dedicated funds for training nurses, and for providing food for patients who cannot afford it. £15 will feed a patient for a month.
If you would like to support the work of Hospice Ethiopia UK, there is more information available on their website hospiceethiopia.org.uk
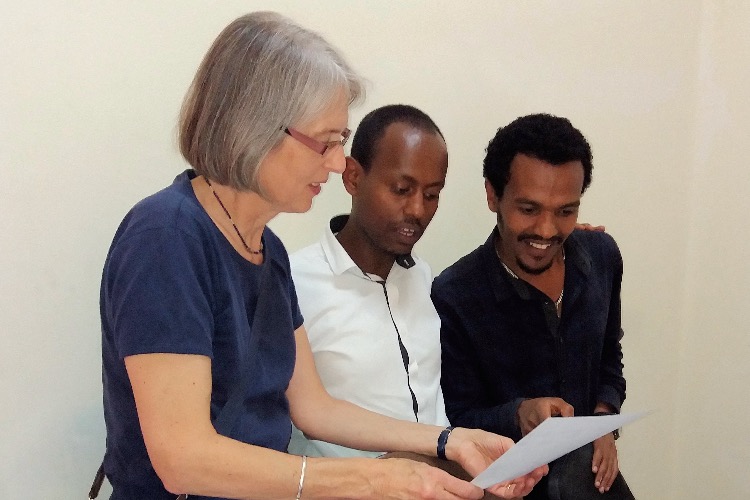
Pictured above are Jamie and Sue Mumford with a patient and, below, Sue with two of the nurses
Eldred Willey, 16/02/2021